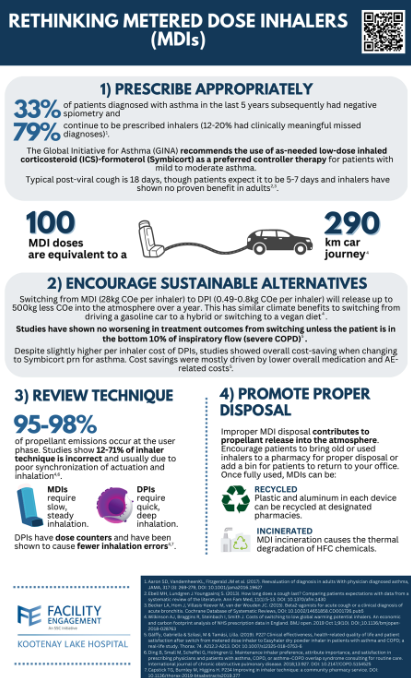
Plans are also underway to engage with the public about the harmful effects of MDIs on our planet. In order to make the transition from an MDI to a DPI as convenient as possible, the working group has composed a letter that will provide permission for pharmacists to switch patients to a DPI upon request. This letter can be faxed to pharmacies once completed and can be accessed here.
If you have any questions about the Engaging in Climate Change at KLH Working Group, or if you would like a printable copy of the infographic below, please contact FE Project Manager Danica Burwash at [email protected]. Dr. Lee MacKay is a family physician, medical director of the diabetes clinic at KLH and a physician lead for the FE Engaging in Climate Change Action Working Group. MacKay is also a proud member of Doctors and Nurses for Planetary Health Kootenay Boundary as well as CASCADES Climate Conscious Inhaler Prescribing C At the recent Facility Engagement Interior Showcase, four stand-out projects from across Interior Health were recognized for excellence in the areas of Achievement, Partnership, Innovation, and Teamwork. Two of these projects were from the Kootenay Boundary; Teamwork –Boundary District Hospital (BDH) for their project Job Description of a Rural Doctor and Partnership–Regional Planetary Health Table. Teamwork –Boundary District Hospital (BDH) for their project Job Description of a Rural Doctor  Pictured from left to right: Dr. Devin Harris (Executive Medical Director, Quality, Engagement and Research), Dr. Max Liu (BDH physician), Tina Hnatiuk (BDH Medical Staff Association), Cindy Myles (Director, Facility and Community Engagement, Doctors of BC), Dr. Andrew Sellars (Senior Medical Director, North Okanagan) In the face of challenges such as hospital staffing shortages, the closure of their inpatient care unit, emergency department crisis, floods, and fires, the Boundary physicians have continued to work together to prioritize meeting the needs of their patients and supporting one another in doing so. The physicians met numerous times to discuss, strategize, and come to a common agreement over what it means to be a physician in the Boundary. They developed documented team processes and agreements about the job requirements of being a rural doctor in the Boundary. This ultimately means working as a team to ensure that the emergency department stays open, long-term care is supported, and medical leadership positions are filled. Partnership – Regional Planetary Health Table  Pictured from left to right: Dr. Devin Harris, Jennifer Brunelle (FE Project Manager, Regional Planetary Health Table), Dr. Kyle Merritt (Kootenay Lake Hospital physician), Danica Burwash (FE Project Manager, Regional Planetary Health Table), Ozora Amin (Environmental Sustainability Coordinator) Cindy Myles, Dr. Andrew Sellars What started as a local Facility Engagement (FE) project related to Climate Action at Kootenay Lake Hospital in Nelson soon grew into the first ever FE funded IH-wide table. This regional table involves physician representation from nine facilities, IH leaders and staff and has gone above and beyond when it comes to collaborating and creating partnerships at both the local and regional level.
This physician-led table has been instrumental in leading quality improvement projects related to environmental sustainability and engaging physicians in the development of Interior Health’s Climate Change and Sustainability Roadmap. At the facility level, pilot projects are in progress around metered-dose inhalers (Kelowna General Hospital and Vernon Jubilee Hospital, in partnership with IH Pharmacy leads) and sustainable perioperative care (Queen Victoria Hospital, Royal Inland Hospital, and East Kootenay Regional Hospital, in partnership with the Surgical Services Network). Efforts to reduce anesthetic gas emissions are also spreading through this table. The table is also aligning priorities with other organizations working in the field of planetary health such as Health Quality BC and CASCADES further demonstrating the positive impact that working together and sharing resources can have on achieving collective goals, and improving health outcomes for all. Emergency Preparedness in the Kootenay Boundary: Ensuring Resilience in the Face of Adversity8/10/2023
In the picturesque region of Kootenay Boundary, nestled amidst stunning landscapes and natural wonders, lies the importance of preparedness in the face of emergencies. From the charming communities of Nelson, Rossland, and Trail to the vast wilderness beyond, the region's beauty and tranquility can sometimes be overshadowed by potential hazards such as wildfires, floods, and other natural disasters. Therefore, it becomes imperative for both residents and professionals to embrace emergency preparedness as an integral part of their lives.
The Kootenay Boundary Division of Family Practice have prepared an Emergency Preparedness Toolkit that provides practical resources to help clinics take a proactive approach to plan and prepare for emergencies such as fire, flood, and internal threats that could impact operations. These resources also support the regular review of established emergency plans and include practice scenarios. The best time to plan for a disaster is before it happens. The Toolkit consists of an Emergency Preparedness Guidebook and accompanying Workbook that includes:
Emergency Management Guidebook for Clinics > Emergency Management Workbook for Clinics > Clinic Poster with Quick Links to these Resources > Emergency preparedness is a fundamental aspect of community safety and resilience. The Kootenay Boundary Division of Family Practice, in close collaboration with local authorities and stakeholders, are actively working towards creating a culture of preparedness, equipping residents with life-saving skills, and ensuring that the region is well-prepared to face any adversity. As residents of the Kootenay Boundary, it is our shared responsibility to embrace emergency preparedness as an integral part of our lives. By understanding the risks, staying informed, and actively participating in preparedness initiatives, we can all contribute to building a safer and stronger community that thrives in the face of challenges. Patient-facing Emergency Preparedness Information If your clinic is interested in information to share with your patients about how they can prepare for potential emergencies, including things your clinic can be doing to support patients, check out what KB Health Online Clinic shares with their patients: kbhealthonline.ca/extreme-weather-preparedness Dr. KYLE MERRITT reflects on DIAGNOSIS OF 'climate change' that BECAME WORLD-WIDE NEWS last year.7/11/2022
Reflecting on it, after a thankfully cool and rainy spring in June, 2022, Dr. Merritt wrote this piece to his colleagues at Kootenay Lake Hospital:
"Last year at this time, we saw an unprecedented number of patients presenting symptoms of acute and subacute heat stress in the KLH emergency department. This trend was attributed to the heat dome that we experienced in Nelson during late June to early July. This high-pressure system trapped hot air in our atmosphere for several days, with temperatures remaining stagnant throughout the evening and nighttime hours. In years prior, temperatures would normally drop off overnight, providing more opportunity for people to cool down. This unusual weather event presented challenges in emergency departments across the Kootenay Boundary. The effects of climate change and the accompanying impacts on community health proved to be unpredictable and unlike anything we had seen before. We had to quickly adapt to the high number of patients that required treatment for heat-related illnesses. In the event that we are faced with a similar event this year, I have included a list of helpful resources at the bottom of this article so that we can be better prepared to handle it. The effects of the heat dome are particularly concerning for seniors and people who are living with mental illness and chronic illness. Medical frailty and social isolation can prevent people from seeking help and being able to cool themselves appropriately. According to the BC Coroners Service, 619 deaths were identified as heat-related between June 25 and July 1, 2021 and were comprised of mostly older adults with existing health concerns who lived alone. Ninety-eight percent of these deaths occurred indoors. The Coroner’s report calls our attention to the number of people in our communities who are isolated and our need as a community to adapt to the extreme weather events we are seeing as a result of climate change. While it is important for us as physicians to address the effects of climate change in relation to health, I would also like to stress that these preventable deaths are a public concern. I hope that these statistics will open the door for more dialogue about heat-related deaths and illness to encourage our community to implement strategies that will keep our most vulnerable members safe during times of extreme heat." Have questions or feedback? Let us know. |
Archives
May 2024
Categories
All
|