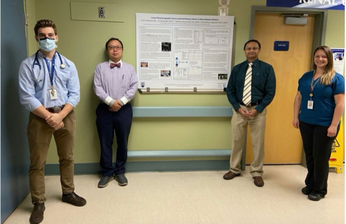
 Justin Dragoman (Medical student), Chi Zhang MD (Chief of Nephrology and the Department of Medicine), Marlene Johnson RN (Dialysis Nurse), and Dharma Paul L. Raju MD (Nephrologist and Project Coordinator) Justin Dragoman (Medical student), Chi Zhang MD (Chief of Nephrology and the Department of Medicine), Marlene Johnson RN (Dialysis Nurse), and Dharma Paul L. Raju MD (Nephrologist and Project Coordinator) Even established medical practices like dialysis can benefit from new approaches. A Kootenay Boundary Regional Hospital team pooled their skills to search for a safe way to remove lung fluids during dialysis treatment. The team followed their hypothesis and analyzed the side effects of fluid retention on hemodialysis patients. Their goal was to see what benefits lung ultrasounds could provide for patients experiencing hypertension during treatment. The Lung Ultrasonographic Assessment of Volume Status in Hemodialysis team was keen to test Point of Care Ultrasound (POCUS) to identify extravascular lung water volume overload. It requires care and accuracy before taking action. “If you remove fluid too excessively, it can precipitate low blood pressure, loss of consciousness, heart attacks,” said DharmaPaul L. Raju MD (Nephrologist and Project Coordinator). “It can be quite dangerous.” Results give new insights and options The team members represented the variety of service providers a dialysis patient might come in touch with during treatment. This Physician Quality Improvement project was conducted by Justin Dragoman (Medical student), Chi Zhang MD (Chief of Nephrology and the Department of Medicine), Marlene Johnson RN (Dialysis Nurse), and Dharma Paul L. Raju MD (Nephrologist and Project Coordinator) at KBRH. The lung ultrasound results demonstrated a statistical decrease in the overall time patients were hypertensive while on dialysis. Also, the ultrasound allowed the researchers to identify patients with sub-clinical congestive heart failure (those without signs or symptoms of heart failure) who benefited from additional fluid removal. Most of the test patients were asymptomatic, leading to improved targeted ultrafiltration (UF) for patients with subclinical volume overload. UBC Medical student Justin Dragoman explained how the first step was to assess how often patients were becoming hypotensive during treatment. “We determined patients spent about 40 percent of their time in hypotension when they are undergoing a dialysis session.” Using lung ultrasound technology helped reduce the patient’s time in hypotension by 12 percent and deal with low blood pressure issues. Looking to the future “As physicians, we want to make sure we improve patient outcomes,” said Chi Zhang MD, Chief of Nephrology and the Department of Medicine. “But also we want to improve their physical well-being and experience with dialysis.” Lung ultrasonography has already been utilized by ICU and Emergency Room physicians. The project plans to expand throughout Interior Health and engage students and nurses throughout the region. Using this simple invaluable bedside tool can enhance patient safety in rural areas without easy access to hospital services. Review this project report here If you want to learn more about this initiative or anything else about living and working as a physician in Kootenay Boundary, please get in touch with Sylvain Turgeon, Head of the KB Doctors Recruitment Team. Like, Share and Follow us @kbdoctors.ca Facebook l Instagram l LinkedIn l Youtube  Dr. Sue Babensee, KBRH Physician and Project Lead. Dr. Sue Babensee, KBRH Physician and Project Lead. Kootenay Boundary Regional Hospital (KBRH) Project Spotlight One thing that was a standard normal for our profession and services became a new normal for our patients in 2020. Masks. But, while many of us are comfortable with masks, and find them necessary and often preferable, for others it is uncomfortable and un-welcome. Wearing masks for safety may have grown in acceptance and practice but at the same time so did an increased desire to see people’s faces. Patients want to see their doctors’ faces. The solution: the Kootenay Boundary Physicians Association (KBPA) Face Button Project. KBPA’s goal is to supply all physicians, nurses, admin staff—anyone working at KBRHs—with their own smiling face button to wear for the public, patients, and colleagues. We are committed to this ‘face time’ project and participation is growing. It's a simple solution to the complex COVID protection protocols. The US National Centre for Biotechnology Information (NCBI) recently reported on the severe affects and challenges wearing face coverings are producing during the pandemic. They explore how “…the face mask can hinder interpersonal communication…”, an important component of our services. A key side-effect of masks is blocking facial expressions critical in comprehension. The facial muscles that create expressions, predominantly moving our nose and mouth, are important when conveying emotions and information. As communication is a two-way street, we are experiencing even more congestion as both parties communicating are wearing masks. The smooth flow of information is prone to being blocked. The KBPA are supporting the #KBRHSmiles to provide a face button with a head and shoulders photo so everyone can see the smile behind your mask. Dr. Sue Babensee, KBRH physician and Project Lead, wears hers with pride, loving the positive response she gets when others see her happy face. We’ve made it easy for KBRH IH Staff and physicians to join in. Take a selfie or chose a photo and contact your department head or our Project Co-Ordinator: [email protected]. The rest is up to us. We’ll send your button and you can join the growing number of project supporters.
Get your smile out from behind your mask. Let’s face it. Putting our real face forward is a prescription for better connections, so important at this time. Date: January 2021 |
Archives
May 2024
Categories
All
|

