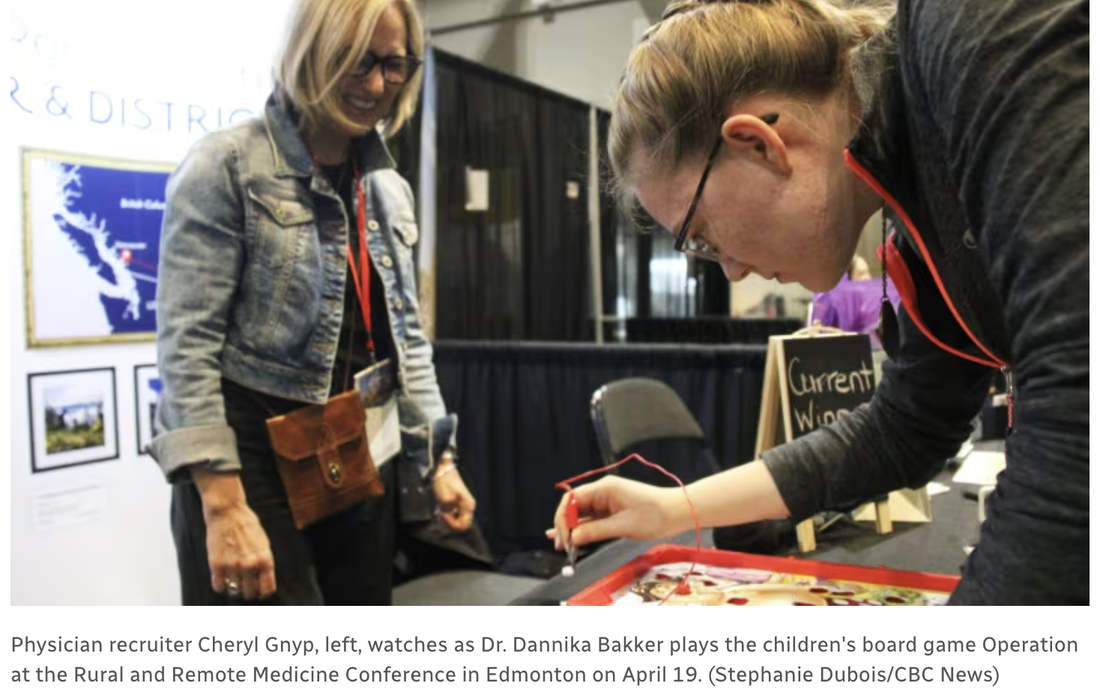
Canada faces a significant challenge in its healthcare system as millions lack access to a family practitioner, a situation exacerbated by a decrease in medical graduates choosing family medicine. In response, recruiters like Cheryl Gnyp from Castlegar, B.C., are employing unique strategies to attract physicians to their communities. Cheryl Gnyp's approach at the Rural and Remote Medicine Conference in Edmonton exemplifies the innovative strategies needed to draw attention amidst the stiff competition from recruiters nationwide. Using the children’s game Operation and specialized coffee, Gnyp crafts a memorable 10-minute sales pitch aimed at potential recruits. This playful yet poignant method not only breaks the ice but also serves as a metaphor for the precision and care required in family medicine. Physician recruitment is not a quick fix but a long-term investment. For Gnyp, attracting a family practitioner to start practicing in Castlegar and the Kootenay Region can take years, reflecting her commitment to the community and understanding of the recruitment landscape. It's a high-stakes endeavor, as each interaction at her booth could lead to securing a family practitioner who will significantly impact the community's health services. Fourth-year medical student Nicole Costanzo's engagement with the Operation game at Gnyp’s booth highlights the interactive and direct approach to attracting younger physicians. By engaging directly with students and residents, Gnyp not only promotes the opportunities in Castlegar and the Kootenays but also invests in the future of rural health care. Read the CBC article: Millions of Canadians need a family doctor. Here’s how one B.C. recruiter attracts them Listen to the interview on White Coat, Black Art: https://www.cbc.ca/listen/live-radio/1-75-white-coat-black-art As recruiters like Cheryl Gnyp continue to stand out with their unique approaches, it is clear that solving the healthcare crisis will require both immediate ingenuity and long-term strategic planning. The efforts in Castlegar serve as a valuable model of commitment and creativity in addressing one of Canada's most pressing healthcare challenges. Source: https://www.cbc.ca/radio/whitecoat/millions-of-canadians-need-a-family-doctor-here-s-how-one-b-c-recruiter-attracts-them-1.7184945 Looking for family practitioner and specialist physician opportunities in Kootenay Boundary visit www.kbdoctors.ca and connect with our recruitment specialists today. Come and try a Locum!
The second day was dedicated to an extensive educational program, welcoming physicians, and specialists from the Kootenay Boundary (KB) region. One of the standout sessions was led by Dr. Paul and Jane Healey, focusing on financial independence. Local experts such as Dr. Lawe, Dr. Merritt, and Dr. Fairbairn captivated participants with insightful discussions on planetary health, general surgery, and advanced ultrasound techniques, encouraging active engagement throughout.  Adding to the excitement, UBC medical students and staff surprised everyone with an impromptu flash mob dance, showcasing their enthusiasm and energy. The unique combination of funky shoes and Dr. Raz's adidas track suits added an extra element of fun to the day. The evening was a celebration of camaraderie and joy as attendees danced to the infectious beats of "Stubbs and the" enjoying over two hours of non-stop music and entertainment.
The following morning offered options for relaxation and adventure, with some attendees opting for discounted tickets to Red Mountain Resort while others enjoyed well-deserved rest and relaxation in the comfort of the hotel's amenities, including the hot tub. Feedback from participants unanimously hailed the event as the best Kootenay Conference to date, a testament to the hard work and dedication of the CPD staff and the invaluable contributions of Dr. Melissa Herr, whose creative ideas and tireless efforts were instrumental in planning and executing a memorable conference experience. We have tentatively set the date for February 27, 28, and Mar 1 2025 for the 41st Kootenay Conference! This will take place in Nelson Bc, and we look forward to Nelson physicians to join the planning team to make next years event even better! Our medical community is growing, and we are recruiting Family Practitioners and Specialists in Kootenay Boundary. Explore the charm of these picturesque mountain towns and envision how your career, family and lifestyle could work in Rossland & Trail, Nelson & Area, Castlegar, Slocan and the Boundary. Looking for physician opportunities in Kootenay Boundary, connect with our recruitment specialists today: Permanent & Locum Family Practice in Kootenay Boundary and Permanent & Locum Positions Kootenay Boundary Regional Hospital. The Kootenay Boundary Patient Advisory Committee & Community (PACC) has launched a campaign titled "Empowering the Citizen Patient," aimed at enhancing community engagement and patient involvement in health care amidst challenges such as a shortage of family practitioners.
The initiative features informative articles, starting with a piece that offers an interactive infographic on navigating the health care system and a compilation of resources for patient support. Future articles will discuss health conditions, mental health, and tips for medical appointments. PACC seeks to amplify patient voices and foster collaborative efforts for health system improvement in the Kootenay Boundary region. QUOTES FROM KOOTENAY BOUNDARY RESIDENTS: “Reading this article is a way for people to get information to ensure that their health care needs are being met,” says Sandi McCreight, resident of Castlegar BC and local seniors advocate and educator. “We need to take charge of this ourselves. Knowledge is power. Once you start reading this information, it leads to more learning. I would encourage people to follow this series and learn as much as they can.” Madeleine Perriere, resident of Slocan says, ” With the knowledge of how the medical system works, we have a better chance to understand and even get involved in improving our health system. This article is clear and informative for us to navigate according to our needs.” “As a Kootenay Boundary resident, understanding the health care system felt like trying to decode a complex puzzle,” says Arlene Parkinson, resident of Warfield, BC. “Although I have been extremely lucky to have a family doctor, many others are struggling in their quest for consistent health care. This article, especially the visual infographic, will help to give more clarity. It’s empowering to know how the system works, and with that knowledge, I feel more confident making informed decisions about my health and that of my community.” WE INVITE YOU TO VISIT: Healthy People, Healthy Communities - What’s Happening in Health Care? to view the first article, infographic and sign up to receive each article as they are published. ABOUT PACC: The Kootenay Boundary Patient Advisory Committee & Community (PACC) is a group of local residents working together as volunteers to bring patient perspectives on important issues to health care providers & policymakers in our region. The PACC works in collaboration with health care partners to help shape improvements that strengthen patient- & family-centred care in our region.
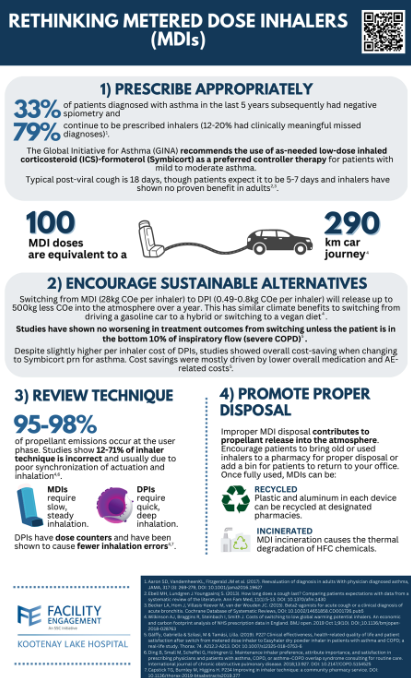
Plans are also underway to engage with the public about the harmful effects of MDIs on our planet. In order to make the transition from an MDI to a DPI as convenient as possible, the working group has composed a letter that will provide permission for pharmacists to switch patients to a DPI upon request. This letter can be faxed to pharmacies once completed and can be accessed here.
If you have any questions about the Engaging in Climate Change at KLH Working Group, or if you would like a printable copy of the infographic below, please contact FE Project Manager Danica Burwash at [email protected]. Dr. Lee MacKay is a family physician, medical director of the diabetes clinic at KLH and a physician lead for the FE Engaging in Climate Change Action Working Group. MacKay is also a proud member of Doctors and Nurses for Planetary Health Kootenay Boundary as well as CASCADES Climate Conscious Inhaler Prescribing C At the recent Facility Engagement Interior Showcase, four stand-out projects from across Interior Health were recognized for excellence in the areas of Achievement, Partnership, Innovation, and Teamwork. Two of these projects were from the Kootenay Boundary; Teamwork –Boundary District Hospital (BDH) for their project Job Description of a Rural Doctor and Partnership–Regional Planetary Health Table. Teamwork –Boundary District Hospital (BDH) for their project Job Description of a Rural Doctor  Pictured from left to right: Dr. Devin Harris (Executive Medical Director, Quality, Engagement and Research), Dr. Max Liu (BDH physician), Tina Hnatiuk (BDH Medical Staff Association), Cindy Myles (Director, Facility and Community Engagement, Doctors of BC), Dr. Andrew Sellars (Senior Medical Director, North Okanagan) In the face of challenges such as hospital staffing shortages, the closure of their inpatient care unit, emergency department crisis, floods, and fires, the Boundary physicians have continued to work together to prioritize meeting the needs of their patients and supporting one another in doing so. The physicians met numerous times to discuss, strategize, and come to a common agreement over what it means to be a physician in the Boundary. They developed documented team processes and agreements about the job requirements of being a rural doctor in the Boundary. This ultimately means working as a team to ensure that the emergency department stays open, long-term care is supported, and medical leadership positions are filled. Partnership – Regional Planetary Health Table  Pictured from left to right: Dr. Devin Harris, Jennifer Brunelle (FE Project Manager, Regional Planetary Health Table), Dr. Kyle Merritt (Kootenay Lake Hospital physician), Danica Burwash (FE Project Manager, Regional Planetary Health Table), Ozora Amin (Environmental Sustainability Coordinator) Cindy Myles, Dr. Andrew Sellars What started as a local Facility Engagement (FE) project related to Climate Action at Kootenay Lake Hospital in Nelson soon grew into the first ever FE funded IH-wide table. This regional table involves physician representation from nine facilities, IH leaders and staff and has gone above and beyond when it comes to collaborating and creating partnerships at both the local and regional level.
This physician-led table has been instrumental in leading quality improvement projects related to environmental sustainability and engaging physicians in the development of Interior Health’s Climate Change and Sustainability Roadmap. At the facility level, pilot projects are in progress around metered-dose inhalers (Kelowna General Hospital and Vernon Jubilee Hospital, in partnership with IH Pharmacy leads) and sustainable perioperative care (Queen Victoria Hospital, Royal Inland Hospital, and East Kootenay Regional Hospital, in partnership with the Surgical Services Network). Efforts to reduce anesthetic gas emissions are also spreading through this table. The table is also aligning priorities with other organizations working in the field of planetary health such as Health Quality BC and CASCADES further demonstrating the positive impact that working together and sharing resources can have on achieving collective goals, and improving health outcomes for all.  In partnership with Red Mountain Ski Resort, Black Jack Ski Club, and Whitewater Ski Resort, and with funding from local medical staff associations, the "Ski Free in KB" campaign aims to attract physicians, locums, nurse practitioners, midwives, medical residents, and students to Kootenay Boundary communities. Eligible medical professionals can look forward to two complimentary days of skiing at each partnering resort as a part of this initiative. "We are incredibly grateful for the steadfast support from Red Mountain Ski Resort, Black Jack Ski Club, and Whitewater Ski Resort," said Kimberley Pegg, SkiFreeinKB campaign manager. "Their contributions are pivotal in helping us showcase the Kootenay Boundary as a place where work-life balance isn't just a phrase but a lifestyle for medical practitioners. It's heartening to see our community come together to welcome medical practitioners and their families, offering them a taste of what makes our region truly exceptional." The Ski Free in KB Campaign serves as a key component of KBDoctors.ca ongoing recruitment strategy. Beyond offering recreational perks, the campaign emphasizes the exceptional lifestyle and opportunities that come with practicing medicine in the Kootenay Boundary Region. The campaign is now in its third year and helps inspire new practitioners to choose the region. Here is what Resident Family Practitioner Dr. Matthew Prisk said about the program: “I thought the KBDoctors.ca SkiFreeinKB Campaign was great! As a visiting resident I thought it was an excellent experience, and I greatly appreciated not only the passes, but the prompt and kind communication. It allowed me to get out and see the area more than I probably would have, and would definitely be a positive influence towards me coming back as a practicing physician when my training is complete.” The recruitment of top-notch medical practitioners to the Kootenay Boundary Region is more than a campaign—it's a community celebration of what makes our region a great place to live and work. While KBDoctors.ca spearheads the Ski Free in KB initiative, its real momentum and success will come from our communities spreading the word. Dr. Carolyn Stark, Head of Psychiatry at KBRH adds, "Please consider this an open invitation to join us in spreading the word! Know a medical practitioner who might be interested? A quick share of the Ski Free in KB campaign or the KBDoctors.ca website could be the nudge they need to make the move to the Kootenays, enriching our community as practitioners and people!" Think about supporting our campaign by sharing and following our posts on KBDoctors.ca Facebook and Instagram. #kbdoctorsskired #kbdoctorsskiwhitewater #kbdoctorsskiblackjack KBdoctors.ca is proud to bring you this guest blog post from Jonathan Vanderhoek, Rural Pre-Medicine Program Coordinator at Selkirk College. The article spotlights the transformative impact of the Selkirk Rural Pre-Medicine Program in fostering the next generation of health professionals dedicated to rural care. The Kootenay Boundary medical community has been a very proud provider of support for the program since 2017.
Located amidst the breathtaking Kootenay mountains, the program offers far more than academic rigor. It combines a robust curriculum with unique opportunities for mentoring and community service, aiming to shape well-rounded professionals suited for a multitude of health science fields. From medicine and pharmacy to optometry, dentistry, and beyond, students in the RPM program are prepared to excel in leadership, resilience, communication, and collaboration. This comprehensive approach ensures they are not just academically prepared but also intrinsically motivated to contribute to the betterment of rural health landscapes. The Kootenay Boundary medical community has provided enduring support for the Selkirk College RPM program over the years, including consulting on program design, making connections in rural health, and presenting to students. Since 2017, the medical community has funded scholarships of $46,500, supporting twenty-five students on their journey towards a career in the medical field from MD Programs to Pharmacy. For example, Jocey Terwoord and Sam Keefer (recipients in 2017) are each in their third year of the MD Program at UBC, with Jocey in the Island Medical Program and Sam in the Northern Medical Program. Rebecca Macleod and Kira Stoochnoff (2018) are in their second year at the Vancouver Fraser Medical Program, while Madison Morehouse (2017) is in her final year. Recipients have also found success on other academic paths. Madia Rehwald (2017) and Gemma van Doesburg (2020) have matriculated into the Doctor of Pharmacy program at UBC. Tia Murdoch (2021) is an Undergraduate Research Assistant at Vancouver General Hospital as she finishes her BSc at UBC. Emily Martin (2018) entered the UBC Law School, Megan Cousins (2021) is completing a degree at UNBC before applying to enter the Masters in Physical Therapy Program, Jace Lamoureux (2021) is completing the UBC Honors Biotechnology program, and Sam Zerrath (2018) is practicing paramedicine. The torch is passed on to this year's deserving recipients: James Lerch, Tayten Dewar (will graduate next spring 2024), and Grace Goodwin, as they embark on their promising journeys in healthcare. Voices of Gratitude: Testimonials from this year’s scholarship recipients Grace Goodwin - 2nd Year Rural Pre-Medicine, Nelson Native "Being born and raised in Nelson has given me a deep appreciation for the healthcare needs of rural communities. Thank you so much for awarding me the Kootenay Boundary Division of Family Practice scholarship. This award is not just financial support; it's a confirmation that I'm on the right path toward serving the healthcare needs of communities like my own." Tayten Dewar - 3rd Year Rural Pre-Medicine, Kootenays Enthusiast "Living my entire life in the Kootenays has made me passionate about health and science, especially in rural settings. Your generosity not only provides invaluable financial support but also reaffirms my dedication to pursuing a career in medicine. This scholarship fuels my aspiration to come back and serve communities like the one I call home." James Lerch - 3rd Year Rural Pre-Medicine, Raised in Passmore B.C. "Growing up in Passmore and experiencing first-hand the challenges of accessing medical care in rural areas has shaped my career goals. This scholarship is more than just monetary assistance; it's a vote of confidence in my potential to bring change to rural healthcare. Your support brings me one step closer to realizing my dream of becoming a rural emergency physician." Emergency Preparedness in the Kootenay Boundary: Ensuring Resilience in the Face of Adversity8/10/2023
In the picturesque region of Kootenay Boundary, nestled amidst stunning landscapes and natural wonders, lies the importance of preparedness in the face of emergencies. From the charming communities of Nelson, Rossland, and Trail to the vast wilderness beyond, the region's beauty and tranquility can sometimes be overshadowed by potential hazards such as wildfires, floods, and other natural disasters. Therefore, it becomes imperative for both residents and professionals to embrace emergency preparedness as an integral part of their lives.
The Kootenay Boundary Division of Family Practice have prepared an Emergency Preparedness Toolkit that provides practical resources to help clinics take a proactive approach to plan and prepare for emergencies such as fire, flood, and internal threats that could impact operations. These resources also support the regular review of established emergency plans and include practice scenarios. The best time to plan for a disaster is before it happens. The Toolkit consists of an Emergency Preparedness Guidebook and accompanying Workbook that includes:
Emergency Management Guidebook for Clinics > Emergency Management Workbook for Clinics > Clinic Poster with Quick Links to these Resources > Emergency preparedness is a fundamental aspect of community safety and resilience. The Kootenay Boundary Division of Family Practice, in close collaboration with local authorities and stakeholders, are actively working towards creating a culture of preparedness, equipping residents with life-saving skills, and ensuring that the region is well-prepared to face any adversity. As residents of the Kootenay Boundary, it is our shared responsibility to embrace emergency preparedness as an integral part of our lives. By understanding the risks, staying informed, and actively participating in preparedness initiatives, we can all contribute to building a safer and stronger community that thrives in the face of challenges. Patient-facing Emergency Preparedness Information If your clinic is interested in information to share with your patients about how they can prepare for potential emergencies, including things your clinic can be doing to support patients, check out what KB Health Online Clinic shares with their patients: kbhealthonline.ca/extreme-weather-preparedness Party Hats On, Dancing Shoes Polished: Dive into the West Kootenay Festivals Frenzy of 2023!7/14/2023
 Welcome to the vibrant world of West Kootenay Festivals 2023, where the air is filled with excitement and the spirit of camaraderie. Join us as we embark on a journey through the diverse range of summertime celebrations that make this region come alive. From mesmerizing music festivals to enchanting nature events and captivating cultural gatherings, there's something for everyone in the Kootenays. These festivals not only bring joy and unity to our community but also contribute to the local economy, attracting visitors from near and far. Festivals Uniting Communities: In the Kootenays, festivals are more than just events; they are experiences that create lasting memories and forge connections. Imagine being surrounded by unfamiliar faces, yet feeling a sense of kinship and togetherness. It's this shared experience that makes festivals so popular and cherished by die-hard festival-goers. A Kaleidoscope of Festivals: Let's explore some of the most prominent festivals throughout the West Kootenay region, where music, nature, and culture intertwine to create unforgettable moments.
Cultural safety is an outcome based on respectful engagement that recognizes and strives to address power imbalances inherent in the health care system. It results in an environment free of racism and discrimination, where people feel safe when receiving health care.1 Cultural humility is a process of self-reflection to understand personal and systemic biases and to develop and maintain respectful processes and relationships based on mutual trust. Cultural humility involves humbly acknowledging oneself as a learner when it comes to understanding another’s experience. 2 Local Indigenous Context In most areas of BC, Indigenous-led health and social services are provided in partnership with or through First Nations or Métis communities, as well as through Aboriginal Friendship Centres. In Kootenay Boundary, the traditional and unceded territory of the Ktunaxa, Secwépemc, Sinixt and Syilx Nations, there are no First Nation Bands or Reserves (the closest band is the Lower Kootenay (Yaqan Nukiy), of the Ktunaxa Nation, located near Creston). There are three chartered Métis Communities within the region, which provide cultural support and connections for Métis people. There is no Aboriginal Friendship Centre in the Kootenay Boundary. There is a dispersed population of Aboriginal peoples living in the region. While Nation members from the unceded traditional territories of the four Nations named above live in Kootenay Boundary, there are also Aboriginal people from a variety of other Nations. With over 600 distinct Nations across Canada’s southern provinces, as well as the Inuit Tapiriit Kanatami, and Dene peoples in the North, it is important to recognize the diversity of cultures and traditions of Aboriginal people. Many local Aboriginal people live away from family and some may be disconnected from their land and cultures. The Circle of Indigenous Nations Society (COINS) is the only Aboriginal-governed and staffed health and social services organization in Kootenay Boundary. It serves a geographically dispersed and culturally diverse Aboriginal population of 6,190 people (Census 2020), a total of 6.4% of the region’s total population. With the introduction of Kootenay Boundary’s Primary Care Network, two Aboriginal Health Coordinators have been hired to support the region’s Indigenous population; they were joined in January 2022 by the Aboriginal Patient Navigator. Become familiar with resources available to Aboriginal peoples to share with your patients. There are Aboriginal patient resources found on the KB Culturally Safety website which you can find HERE. In addition, the Aboriginal Health Team at COINS can be a fantastic resource for yourself and Aboriginal patients. Click the button to download your *Cultivating Cultural Safety in Your Clinic Toolkit for Kootenay Boundary Practitioners *Prepared by the KB Cultural Safety Working Group, with the support of Kootenay Boundary Division of Family Practice, Kootenay Boundary Aboriginal Services Collaborative, and Circle of Indigenous Nations Society Practice, Kootenay Boundary Aboriginal Services Collaborative, and Circle of Indigenous Nations Society Produced April 2022. kbculturalsafety.org is a resource hub for Kootenay Boundary practitioners. Here you will find an inventory of patient resources, filterable by nation, for practitioners to use in helping patients to find the health care supports they need for themselves, and/or their family. For further hands-on support, practitioners can also refer patients to one of Kootenay Boundary’s Aboriginal Health Coordinators using this referral form: https://coinations.net/referral-form-for-aboriginal-health-coordinator/. _________________________ 1. Creating a Climate for Change, First Nations Health Authority 2. Creating a Climate for Change, First Nations Health Authority |
Archives
May 2024
Categories
All
|